
Karthikeyan T
Physiotherapist, NIMHANS, Bangalore, India
*Corresponding Author: Karthikeyan T, Physiotherapist, NIMHANS, Bangalore, India
Received date: September 10, 2021
Accepted date: September 22, 2021
Published date: September 24, 2021
Citation: Karthikeyan T. “Therapeutic Effects of Ultra- Sound and Active Chin Tucking Exercise versus Sub Occipital Muscle Release in Mechanical Mechanical neck pain’’. J Orthopaedic Research and Surgery, 2(4); DOI: http;//doi.org/03.2021/1.1021.
Copyright: © 2021 Karthikeyan T. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Mechanical neck pain is defined as pain in the anatomical region of the neck with sixty percent of the population suffering with it at some point in their lives. It is a common can be caused by many other spinal problems. Mechanical neck pain may arise due to muscular tightness in both the neck and upper back, and pinching of the nerves emanating from the cervical spine. It is the most common one. The causes may be minor strains and sprains to muscles or ligaments in the neck. The objectives Study to investigate therapeutic effects ultra- sound therapy with active chin tucking exercise versus sub occipital muscle release for mechanical neck pain. The outcome used in the study in visual analog scale and copenhagen neck function disability scale. The Methods used in 20 subjects with MNP were included in this study by purposive sampling and randomly assigned to two groups A and B with each group consisting of 10 subjects. The group A was treated with Ultrasound Therapy with Active Chin Tucking Exercises and Group B was treated with Ultrasound Therapy with Sub Occipital Muscle Release Technique. Pain and Neck Function were assessed before and after the intervention by Visual Analog scale and Copenhagen Neck he Function Disability Scale. The Results shows that the Group A Baseline VAS score is 7.4 and post VAS score is4.3. Group B Baseline VAS score is 7.15 and post VAS score is 2.85. Group A Baseline Neck function score is 17.8 and post Neck function score is 9.9. Group B Baseline Neck function score is14.6 and post Neck function score is5.1. This study concluded that Ultrasound Therapy and Active Chin Tucking Exercise help to reduce neck for management of mechanical neck pain.
Introduction:
Mechanical neck pain is defined as pain in the anatomical region of the neck with sixty percent of the population suffering with it at some point in their lives [1]. Mechanical neck pain, although felt in the neck, can be caused by many other spinal problems. Mechanical neck pain may arise due to muscular tightness in both the neck and upper back, and pinching of the nerves emanating from the cervical spine. Mechanical neck pain is the most common one [2]. This is also known as 'simple' or “Non-Specific Mechanical neck pain. The causes may be minor strains and sprains to muscles or ligaments in the neck. Bad posture seems to be the major contributing factor in many cases. Mechanical mechanical neck pain can be caused due to many other physical and emotional health problems as well [3].
Mechanical neck pain is more common in people who spend most of their day working at a desk, in front of the computer with a 'bent-forward' posture or ‘forward head carriage’ posture. Mechanical neck pain is most often caused by continuous forward head carrying posture leading to sub-occipital muscle tightness, decreased cervical mobility and obliterated cervical spine curvature. Forward head posture is commonly adopted by visual display terminal [VDT] workers involving a combination of lower cervical flexion and upper cervical extension. The important causes of forward head posture are improperly placed computer screen, looking down while typing or reading, sitting improperly with shoulders rounded and back hunched, slouched postures or end result of faulty pelvic and lumbar spine posture [4].
In upper cervical spine, flexion and extension both occur at the atlanto-axial region and atlanto-occipital region. The atlanto-occipital region has greater range of motion compared to atlanto-axial region. Flexion in occiput on the atlas is limited by bony contact between anterior rim of foramen magnum and superior surface of dens. The extension is limited by connective tissue restraints of the tectorial and atlanto occipital membrane. The centre of rotation between C1 and C2 falls in the region of dens. The dens closely nestled within the anterior arch of the atlas and surrounded by transverse ligament provide stability and checks the excessive flexion and extension movement. Few degrees of rotation also occur between occiput and atlas. The shape of bony articulations and alar ligament provide rotation and prevents excessive rotation. The inferior articular process of the atlas and superior articular surface of the axis are flat to convex. The articular surface provides opportunity for rotatory motion located in the dens. The rotatory motion of C1 and C2 is coupled to a vertical translation of the same two vertebrae. The head is supported by the lower neck and upper back, and it is these areas that commonly cause mechanical neck pain. The first three joints in the neck allow for most movement of the neck and head. The lower joints in the neck and those of the upper back create a supportive structure for the head to sit on. If this support system is affected, then the muscles in the area will become tight, causing mechanical neck pain.
Various structures involved in transmitting pain in the cervical spine include Facet joints, Inter-vertebral discs, Nerve roots, Ligaments, Fascia, and Muscles. In pathomechanics of upper cervical spine musculature, the rectus capitis posterior minor, the superior oblique, rectus capitis posterior major and inferior oblique muscles are innervated by the dorsal ramus of C1 (sub-occipital nerve) which exits from sub-occipital triangle superior to the arch of atlas. It is primarily a motor nerve but can have cutaneous branch that may result in pain if stretched or tapped. The sub- occipital muscles are deep and difficult to palpate. Several layers of large muscles and dense fascia are interposed between skin and these muscle groups. The location of the symptoms is usually bilateral; pain begins in the neck and spreads to sub-occipital region (area just below the posterior hair line). Tenderness will be present in neck extensors and sub-occipital muscles, neck stiffness, and restriction of neck movements and is diagnosed by mobility test and palpation of the upper cervical spine region for tenderness. A constant forward head posture reduces the average length of the rectus capitis posterior minor, the superior oblique, rectus capitis posterior major and inferior oblique muscles. It contributes to the development of chronic mechanical neck pain. Pain associated with muscle tightness in this area is due to the result of postural problems. The patient with a marked forward head and kyphotic upper thoracic region has a compensatory hyper extension of cervical spine and head. This position leads to tightening and subsequent shortening of the sub-occipital muscles and stretch weakness of anterior neck muscles. The mechanism of pain would be an abnormally large compression force on the articular facet due to altered and sustained pull of the shortened muscles [6].
Forward head posture is the anterior positioning of the cervical spine. In this position, head is slightly leaning forward which causes strain in cervical joints and muscles. There will be flexion in lower cervical region and extension in upper cervical region. It is a long process brought about by constant and repetitive motion, where the head is leaning to the front. For every inch the head moves forward, it gains 10 pounds in weight as far as the muscles in neck and upper back are concerned because they had to work that much harder to keep head from dropping into the chest [5].
Management of Mechanical neck pain due to Sub occipital Muscle tightness includes active chin tucking exercises, ultrasound therapy, stretching, and mobilization of upper cervical muscles. Postural training is commonly used to treat poor posture and cervical dysfunction and involves exercises that are performed repeatedly within pain free range to stretch tightened structures and strengthen weak muscles [7].
Ultrasound Therapy is a method of treating tissue beneath the skin's surface using sound waves [8]. A 1MHz ultrasound will penetrate about 4" below the skin. Both the thermal and Non-thermal effects of the ultrasound are used to treat protective muscle spasm and pain. The increase in tissue temperature due to the therapy reduces the muscle spasm which causes pain in the region (11). This also helps in increasing the extensibility of the tissues due to the reduction in spasm [9].
Stretching is therapeutic maneuver designed to lengthened or elongate pathologically shortened soft tissues and thereby increase range of motion.Stretching techniques are used to increase the extensibility of the muscle tendon unit and the peri-articular connective tissue. Stretching is used to increase the flexibility. Self-Stretching is also referred to as flexibility exercise or active stretching exercises [10].
Objectives:
To investigate the therapeutic effects of ultra- sound and active chin tucking exercise versus sub occipital muscle release in mechanical neck pain
Methodology:
Study Design:
Pre-test Post-test Experimental Design, comparative in nature.
Study Setting:
This study was conducted at Physiotherapy centre, NIMHANS Bangalore, Karnataka.
Study Duration:
The study was conducted for a period of 7 days.
Selection of Subjects:
20 computer professionals aged between 22 and 30 years who fulfilled inclusion and exclusion criteria were selected by purposive sampling method and randomly assigned to two groups of 10 subjects each. Group A was assigned for Ultrasound Therapy with Active Chin Tucking Exercises and Group B for Ultrasound Therapy with Sub Occipital Muscle Release Technique.
Criteria:
Inclusion Criteria:
Exclusion Criteria:
Independent Variable:
Dependent Variable:
Outcome:
Measurement procedure:
Visual Analog scale:
The Visual Analog scale is a measurement tool that measures a characteristic or attitude which ranges across a continuum of values and cannot easily be directly measured.
Operationally VAS is a horizontal line, 10 cm in length, anchored by word descriptors at each end, as illustrated in Fig: 1. The subject marks on the line a point that they feel represents their perception of their current state of pain. The VAS score is determined by measuring in millimeters from the left-hand end of the line to the point that the subject marks.

No Pain Severe Pain
Figure 1: shows the Visual Analog scale –VAS (Not to actual scale)
Copenhagen Neck Function Disability Scale:
The Copenhagen Neck Function Disability Scale is used to evaluate the disability experienced by patients with mechanical neck pain. The scores can be monitored over time to evaluate the disease course and response to any intervention. It is set of 15 questions which rates as 0, 1 and 2 based on their ability and disability. The disability index is the sum of all the scores, where the higher ratings imply greater disability.
Both Group A and Group B subjects were involved in pre-test and post-test assessment by Visual Analog Scale and Copenhagen Neck Function Disability Scale.
Treatment procedure Volume of Training
20 minutes per session 1 session per day
Total number of sessions 7
Treatment Procedure for Group an Ultrasound therapy
Position of the Subject: Sitting in front of a couch and bending the head forward and leaning over the pillows placed on the couch.
Position of Therapist: Standing behind the Subject.
Procedure: 1 MHz pulsed ultrasound with 1.0 watts/cm2 intensity was given on the sub-occipital region for 4 minutes duration.

Picture 1: Researcher giving Ultrasound Therapy
Active Chin Tucking Exercises:
Position of the Subject: High Sitting on the couch:
Position of Therapist: Standing next to the subject viewing the lateral aspect. Procedure: The subject is asked to retract the neck into proper posture aligning the head over the shoulder and then asked to pull the neck slightly up and the chin slightly down to place the neck in cranio-cervical flexion. There is a little head nodding motion as if the subject is nodding "yes" and the chin pulls towards the neck and the back of the head arches slightly up. This causes a stretching sensation at the base of the skull. The subject is asked to perform this exercise 30 times in one session with a hold of 20 seconds each time and a rest interval of 30 seconds after every 10 times (Carolyn Kisner and Lynn Allen Colby, 2007).
Picture 2: Researcher teaching starting position of Active Chin Tucking Exercise

Picture 3: Researcher taching ending position of Active Chin Tucking Exercise
Treatment Procedure for Group B Ultrasound therapy
Position of the Subject: Sitting in front of a couch and bending the head forward and leaning over the pillows placed on the couch.
Position of Therapist: Standing behind the Subject.
Procedure: 1 MHz pulsed ultrasound with 1.0 watts/cm2 intensity was given on the sub-occipital region for 4 minutes duration.
Sub Occipital Muscle Release Technique
Position of the Subject: Supine lying on the couch.
Position of Therapist: Standing at the head end of the supine lying subject.
Procedure: The therapist places both his palms under the head of the subject, reaching the posterior arch of the atlas (C1) just caudal to the superior nuchal line on the sub occipital region with his curled-up fingers and places an upward pressure causing a stretch and distraction for 30 seconds, until tissue relaxation has been achieved. This technique was performed 3 times in one session with a rest interval of 1 minute after each time (Carolyn Kisner and Lynn Allen Colby, 2007).

Picture 4: Researcher performing Sub Occipital Muscle Release Technique
|
Measurement |
Mean |
Mean Difference |
Standard Deviation |
Paired ‘t’ value |
|
Pre-test
Post-test |
7.4
4.3 |
3.1 |
0.27 |
36.28 |
Table 1: Pain in Group A Table showing Mean value, Mean Difference, Standard Deviation and Paired‘t’ value between pre and post test scores of Pain among Group A.
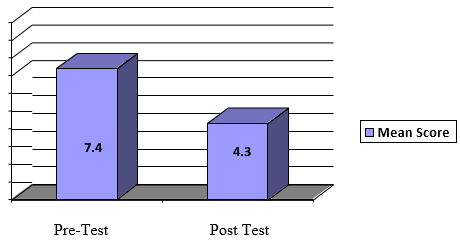
Graph 1: Bar diagram showing the pre and posttest mean values of Pain on Visual Analog Scale among Group A.
|
Measurement |
Mean |
Mean Difference |
Standard Deviation |
Paired ‘t’ value |
|
Pre test
post test |
7.15
2.85 |
4.3 |
0.23 |
59.08 |
Table 2: Pain in Group B. Table showing Mean value, Mean Difference, Standard Deviation and Paired‘t’ value between pre and post test scores of Pain among Group B.
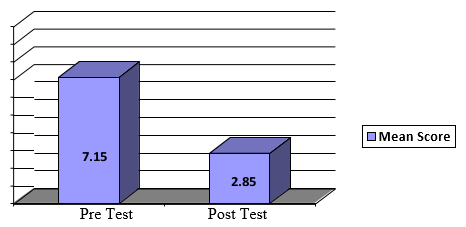
Graph 2: Bar diagram showing the pre and post test mean values of Pain on Visual Analog Scale among Group B.
|
S.NO |
GROUPS |
IMPROVEMENT |
STANDARD DEVIATION |
UNPAIRED ‘T’ TEST |
|
|
1
2 |
GROUP-A
GROUP-B |
Mean |
Mean Difference |
1.2 |
2.23 |
|
3.1
4.3 |
1.2 |
||||
Table 3: Comparison of Pain between Group A and Group B. Table showing Mean value, Mean Difference, Standard Deviation, and Unpaired‘t’ Value scores between Group A and Group B.
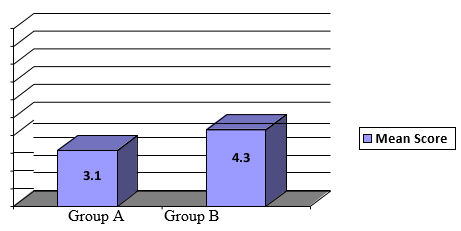
Graph 3: Bar diagram showing Mean values of Pain on Visual Analog Scale in Group A and Group B.
|
Measurement |
Mean |
Mean Difference |
Standard Deviation |
Paired ‘t’ value |
|
Pretest
post test |
17.8
9.9 |
7.9 |
1.23 |
20.29 |
Table 4: Neck Function in Group A. Table Showing Mean value, Mean Difference, Standard Deviation and Paired‘t’ value between pre and post test scores of Neck Function among Group A.
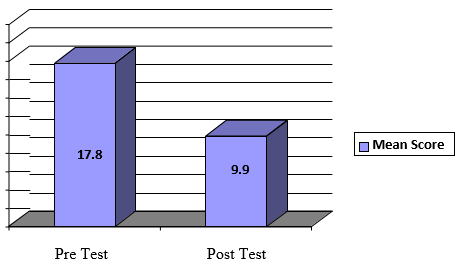
Graph 4: Bar diagram showing the pre and post test mean values of Neck Function on Copenhagen Neck Function Disability Scale among Group A
|
Measurement |
Mean |
Mean Difference |
Standard Deviation |
Paired ‘t’ value |
|
Pre test
post test |
14.6
5.1 |
9.5 |
0.94 |
31.93 |
Table 5: Neck Function in Group B. Table showing Mean value, Mean Difference, Standard Deviation and Paired‘t’ value between pre and post test scores of Neck Function among Group B.
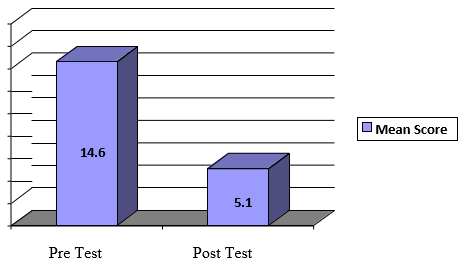
Graph 5: Bar diagram showing the pre and post test mean values of Neck Function on Copenhagen Neck Function Disability Scale among Group B.
|
S.NO |
Groups |
Improvement |
Standard Deviation |
unpaired “t” test |
|
|
1
2 |
Group-A
Group-B |
Mean |
Mean Difference |
3.5 |
1.0 |
|
7.9
9.5 |
1.6 |
||||
Table 6: Comparison of Neck Function between Group A and Group B.
Table showing Mean value, Mean Difference, Standard Deviation, and Unpaired‘t’ Value scores between Group A and Group B.
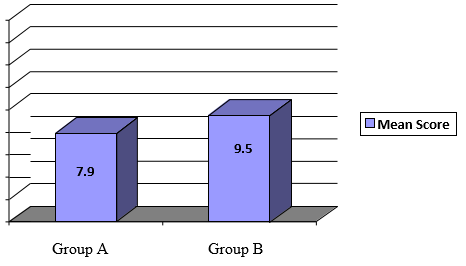
Graph 6: Bar diagram showing Mean values of Neck Function on Copenhagen Neck Function Disability Scale in Group A and Group B.
Discussion:
Non-Specific Mechanical neck pain is common among computer professionals because of as their faulty forward head posture while working on computers, which in turn places constant extension of the upper cervical structures causing tightness of the soft tissues in that area [12].
Studies of Jordan Miller, et al, (2010) shows that mobilization, manipulation and soft tissue techniques decreases pain and improve satisfaction in mechanical neck pain patients. The stretching of Sub occipital muscle influenced pain when combined with other treatment techniques/ modalities in the management of mechanical neck pain in patients with cervicogenic headache [11]. Manual therapy with home program of active neck retraction (Chin Tucking) exercises in a series of progressions was successful in relieving cervicogenic headache and improving neck function [13]. This study concluded that ultrasound therapy is helpful in treating Mechanical Mechanical neck pain.
The purpose of this study is to validate and compare the effects of combination of Ultrasound Therapy with Active Chin Tucking Exercise and combination of Ultrasound therapy with Sub occipital Release Technique on Pain and Neck Function among computer professionals.
The results of the present study indicate that the combination of Ultrasound therapy with Active Chin Tucking Exercise reduces pain and improves neck function as well, thereby validating the study of Hanten, et al. (2005). Whereas the combination of Ultrasound therapy with sub occipital Muscle Release technique reduces only pain and has no significant effect on the neck function among computer professionals having Mechanical Mechanical neck pain, which is similar to the results [14].
Discussion:
Ultrasound therapy with Active Chin Tucking Exercise in reducing Pain and improving Neck Function among computer professionals having Non-Specific Mechanical neck pain.
This study shows that there is significant difference in reducing Pain and improving Neck Function following Ultrasound therapy with Active Chin Tucking Exercises. Therapeutic form of Ultrasound therapy with Sub occipital Muscle Release Technique in reducing Pain and improving Neck Function having Mechanical Mechanical neck pain.
This study shows that there is significant difference in reducing Pain and improving Neck Function following Ultrasound therapy with Sub Occipital Muscle Release Technique. there is no significant difference between Ultrasound therapy with Active Chin Tucking Exercise and Ultrasound therapy with Sub occipital Muscle Release Technique in reducing Pain Neck Function having Mechanical Mechanical neck pain.
This study shows that there is significant difference between Ultrasound therapy with Active Chin Tucking Exercises and Ultrasound therapy with Sub Occipital Muscle Release Technique in reducing Pain Neck Function having Mechanical Mechanical neck pain.
There is no significant difference between Ultrasound therapy with Active Chin Tucking Exercise and Ultrasound therapy with Sub occipital Muscle Release Technique in improving Neck Function having mechanical Mechanical neck pain.
This study shows that there is no significant difference between Ultrasound therapy with Active Chin Tucking Exercises and Ultrasound therapy with Sub Occipital Muscle Release Technique in improving Neck function for the mechanical neck pain.
Conclusion:
This study concluded that there is reduction of pain treated with ultrasound Therapy and Active Chin Tucking Exercise for their mechanical neck pain and also improvement in Neck function It is concluded that there is reduction of pain treated with Ultrasound Therapy and Sub Occipital Muscle Release Technique for their mechanical neck pain.
This study report identified the combination of Ultrasound Therapy with Active Chin Tucking Exercise training showed statistically significant improvement in neck function than the other group. This specific protocols which help to increase quality of life,well being overall health for the management of mechanical neck pain